|
Office of
Disease Prevention and Health Promotion Health Communication Activities |
Ths Guide contains:
A basic overview of key health literacy concepts
Techniques for improving health literacy through communication, navigation, knowledge-building, and advocacy
Examples of health literacy best practices
Suggestions for addressing health literacy in your organization
These tools can be applied to healthcare delivery, policy, administration, communication, and education activities aimed at the public. They also can be incorporated into mission, planning, and evaluation at the organizational level.
If you are new to health literacy, the toolkit will give you the information you need to become an effective advocate for improved health literacy. If you are already familiar with the topic, you will find user-friendly, action-oriented materials that can be easily referenced, reproduced, and shared with colleagues.
The guide is designed to be a quick and easy reference, filled with facts, definitions, helpful tips, checklists, and resources you can use on the job. You can print out the materials and keep them at your desk, share them with colleagues, or bookmark this Web page on your computer.
The Quick Guide is divided into the following three sections:
The first section contains a series of fact sheets on health literacy, including a basic overview of key concepts and definitions and information on health literacy and health outcomes.
- Improve the usability of health information
- Improve the usability of health services
- Build knowledge to improve decisionmaking
- Advocate for health literacy in your organization
The final section contains a list of resources, including Web sites, research studies, and additional publications on health literacy.
| Health Literacy Basics |
What is health literacy?Health literacy is the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.1 Health literacy is dependent on individual and systemic factors:
Health literacy affects people's ability to:
Health literacy includes numeracy skills. For example, calculating cholesterol and blood sugar levels, measuring medications, and understanding nutrition labels all require math skills. Choosing between health plans or comparing prescription drug coverage requires calculating premiums, copays, and deductibles. In addition to basic literacy skills, health literacy requires knowledge of health topics. People with limited health literacy often lack knowledge or have misinformation about the body as well as the nature and causes of disease. Without this knowledge, they may not understand the relationship between lifestyle factors such as diet and exercise and various health outcomes. Health information can overwhelm even persons with advanced literacy skills. Medical science progresses rapidly. What people may have learned about health or biology during their school years often becomes outdated or forgotten, or it is incomplete. Moreover, health information provided in a stressful or unfamiliar situation is unlikely to be retained. What is literacy?Literacy can be defined as a person's ability to read, write, speak, and compute and solve problems at levels necessary to:
The term “illiteracy” means being unable to read or write. A person who has limited or low literacy skills is not illiterate. What is plain language?Plain language is a strategy for making written and oral information easier to understand. It is one important tool for improving health literacy. Plain language is communication that users can understand the first time they read or hear it. With reasonable time and effort, a plain language document is one in which people can find what they need, understand what they find, and act appropriately on that understanding.3 Key elements of plain language include:
Language that is plain to one set of readers may not be plain to others.3 It is critical to know your audience and have them test your materials before, during, and after they are developed. Speaking plainly is just as important as writing plainly. Many plain language techniques apply to verbal messages, such as avoiding jargon and explaining technical or medical terms. What is cultural and linguistic competency?Culture affects how people communicate, understand, and respond to health information. Cultural and linguistic competency of health professionals can contribute to health literacy. Cultural competence is the ability of health organizations and practitioners to recognize the cultural beliefs, values, attitudes, traditions, language preferences, and health practices of diverse populations, and to apply that knowledge to produce a positive health outcome.4 Competency includes communicating in a manner that is linguistically and culturally appropriate.5 Healthcare professionals have their own culture and language. Many adopt the “culture of medicine” and the language of their specialty as a result of their training and work environment. This can affect how health professionals communicate with the public. For many individuals with limited English proficiency (LEP), the inability to communicate in English is the primary barrier to accessing health information and services. Health information for people with LEP needs to be communicated plainly in their primary language, using words and examples that make the information understandable. Why is health literacy important?Only 12 percent of adults have Proficient health literacy, according to the National Assessment of Adult Literacy. In other words, nearly nine out of ten adults may lack the skills needed to manage their health and prevent disease. Fourteen percent of adults (30 million people) have Below Basic health literacy. These adults were more likely to report their health as poor (42 percent) and are more likely to lack health insurance (28 percent) than adults with Proficient health literacy.6 Low literacy has been linked to poor health outcomes such as higher rates of hospitalization and less frequent use of preventive services (see Fact Sheet: Health Literacy and Health Outcomes). Both of these outcomes are associated with higher healthcare costs. Who is at risk?Populations most likely to experience low health literacy are older adults, racial and ethnic minorities, people with less than a high school degree or GED certificate, people with low income levels, non-native speakers of English, and people with compromised health status.7 Education, language, culture, access to resources, and age are all factors that affect a person's health literacy skills. Who is responsible for improving health literacy?The primary responsibility for improving health literacy lies with public health professionals and the healthcare and public health systems. We must work together to ensure that health information and services can be understood and used by all Americans. We must engage in skill building with healthcare consumers and health professionals. Adult educators can be productive partners in reaching adults with limited literacy skills.
1U.S. Department of Health and Human Services. 2000. Healthy People 2010. Washington, DC: U.S. Government Printing Office. Originally developed for Ratzan SC, Parker RM. 2000. Introduction. In National Library of Medicine Current Bibliographies in Medicine: Health Literacy. Selden CR, Zorn M, Ratzan SC, Parker RM, Editors. NLM Pub. No. CBM 2000-1. Bethesda, MD: National Institutes of Health, U.S. Department of Health and Human Services. 2Public Law 102-73. The National Literacy Act of 1991. 3Plain Language Action and Information Network. What Is Plain Language? Available at www.plainlanguage.gov. Accessed on October 21, 2005. 4U.S. Department of Health and Human Services. 2001. National Standards for Culturally and Linguistically Appropriate Services in Health Care. Washington, DC: Office of Minority Health. 5McKinney J, Kurtz-Rossi S. 2000. Culture, Health, and Literacy: A Guide to Health Education Materials for Adults With Limited English Skills. Boston, MA: World Education. 6Kirsch IS, Jungeblut A, Jenkins L, Kolstad A. 1993. Adult Literacy in America: A First Look at the Results of the National Adult Literacy Survey (NALS). Washington, DC: National Center for Education Statistics, U.S. Department of Education. 7National Center for Education Statistics. 2006. The Health Literacy of America's Adults: Results From the 2003 National Assessment of Adult Literacy. Washington, DC: U.S. Department of Education. |
||
| Health Literacy Basics |
|
Choosing a healthy lifestyle, knowing how to seek medical care, and taking advantage of preventive measures require that people understand and use health information. The ability to obtain, process, and understand health information needed to make informed health decisions is known as health literacy. Given the complexity of the healthcare system, it is not surprising that limited health literacy is associated with poor health. This fact sheet summarizes key research study findings on the relationship between health literacy and health outcomes. Use of preventive servicesAccording to research studies, persons with limited health literacy skills are more likely to skip important preventive measures such as mammograms, Pap smears, and flu shots.1 When compared to those with adequate health literacy skills, studies have shown that patients with limited health literacy skills enter the healthcare system when they are sicker.2 Knowledge about medical conditions and treatmentPersons with limited health literacy skills are more likely to have chronic conditions and are less able to manage them effectively. Studies have found that patients with high blood pressure,3 diabetes,3-5 asthma,6 or HIV/AIDS7-9 who have limited health literacy skills have less knowledge of their illness and its management. Rates of hospitalizationLimited health literacy skills are associated with an increase in preventable hospital visits and admissions.10-13 Studies have demonstrated a higher rate of hospitalization and use of emergency services among patients with limited literacy skills.12 Health statusStudies demonstrate that persons with limited health literacy skills are significantly more likely than persons with adequate health literacy skills to report their health as poor.10, 12 14 Healthcare costsPersons with limited health literacy skills make greater use of services designed to treat complications of disease and less use of services designed to prevent complications.1, 11-13 Studies demonstrate a higher rate of hospitalization and use of emergency services among patients with limited health literacy skills.10-13 This higher use is associated with higher healthcare costs.15 16, Stigma and shameLow health literacy may also have negative psychological effects. One study found that those with limited health literacy skills reported a sense of shame about their skill level.17 As a result, they may hide reading or vocabulary difficulties to maintain their dignity.18
1Scott TL, Gazmararian JA, Williams MV, Baker DW. 2002. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Medical Care. 40(5): 395-404. 2Bennet CL, Ferreira MR, Davis TC, Kaplan J, Weinberger M, Kuzel T, Seday MA, Sartor O. 1998. Relation between literacy, race, and stage of presentation among low-income patients with prostate cancer. Journal of Clinical Oncology. 16(9): 3101-3104. 3Williams MV, Baker DW, Parker RM, Nurss JR. 1998. Relationship of functional health literacy to patients' knowledge of their chronic disease. A study of patients with hypertension and diabetes. Archives of Internal Medicine. 158(2): 166-172. 4Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, Palacios J, Sullivan G, Bindman AB. 2002. Association of health literacy with diabetes outcomes. Journal of the American Medical Association. 288(4): 475-482. 5Schillinger D, Grumbach K, Wang F, Wilson C, Daher C, Leong-Grotz K, Castro C, Bindman AB. 2003. Closing the loop: Physician communication with diabetic patients who have low health literacy. Archives of Internal Medicine. 163(1): 83-90. 6Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. 1998. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest. 114(4): 1008-1015. 7Kalichman SC, Ramachandran BB, Catz SP. 1999. Adherence to combination antiretroviral therapies in HIV patients of low health literacy. Journal of General Internal Medicine. 14(5): 267-273. 8Kalichman SC, Rompa D. 2000. Functional health literacy is associated with health status and health-related knowledge in people living with HIV-AIDS. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 25(4): 337-344. 9Kalichman SC, Benotsch E, Suarez T, Catz S, Miller J, Rompa D. 2000. Health literacy and health-related knowledge among persons living with HIV/AIDS. American Journal of Preventive Medicine. 18(4): 325-331. 10Baker DW, Parker RM, Williams MV, Clark WS. 1997. The relationship of patient reading ability to self-reported health and use of health services. American Journal of Public Health. 87(6): 1027-1030. 11Baker DW, Parker RM, Williams MV, Clark WS. 1998. Health literacy and the risk of hospital admission. Journal of General Internal Medicine. 13(12): 791-798. 12Baker DW, Gazmararian JA, Williams MV, Scott T, Parker RM, Green D, Ren J, Peel J. 2002. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. American Journal of Public Health. 92(8): 1278-1283. 13Gordon MM, Hampson R, Capell HA, Madhok R. 2002. Illiteracy in rheumatoid arthritis patients as determined by the Rapid Estimate of Adult Literacy (REALM) score. Rheumatology. 41(7): 750-754. 14National Center for Education Statistics. 2006. The Health Literacy of America's Adults: Results from the 2003 National Assessment of Adult Literacy. Washington, D.C.: U.S. Department of Education. 15Friedland R. 1998. New estimates of the high costs of inadequate health literacy. In: Proceedings of Pfizer Conference “Promoting Health Literacy: A Call to Action.” October 7-8, 1998, Washington, DC: Pfizer, Inc., 6-10. 16Howard DH, Gazmararian J, Parker RM. 2005. The impact of low health literacy on the medical costs of Medicare managed care enrollees. The American Journal of Medicine, 118, 371-377. 17Parikh NS, Parker RM, Nurss JR, Baker DW, Williams MV. 1996. Shame and health literacy: The unspoken connection. Patient Education and Counseling. 27(1): 33-39. 18Baker DW, Parker MR, Williams MV, Ptikin K, Parikh NS, Coates W, Imara M. 1996. The health care experience of patients with low literacy. Archives of Family Medicine, 5(6): 329-334. |
||||||||||||||||
Be sure the materials and messages reflect the age, social and cultural diversity, language, and literacy skills of the intended users. Consider economic contexts, access to services, and life experiences.1 Beyond demographics, culture, and language, consider the communication capacities of the intended users. Approximately one in six Americans has a communication disorder or difference resulting in unique challenges.2 These individuals will require communication strategies that are tailored to their needs and abilities. Evaluate users' understanding before, during, and after the introduction of information and services.Talk to members of the intended user group before you design your communication intervention to determine what information they need to know and how they will use it. Then, pretest messages and services to get feedback. Test your messages again, after they have been introduced, to assess effectiveness. Refine content when necessary. Use a post-test to evaluate the effectiveness of the information. Acknowledge cultural differences and practice respect.Cultural factors include race, ethnicity, language, nationality, religion, age, gender, sexual orientation, income level, and occupation. Some examples of attitudes and values that are interrelated with culture include:
Ensure that health information is relevant to the intended users' social and cultural contexts.
|
||||||||||||||||
| For print communication, use captions or cues to point out key information.3 Show the main message on the front of the materials. |
Make written communication look easy to read.3-5
Use at least 12-point font. Avoid using all capital letters, italics, and fancy script. Keep line length between 40 and 50 characters. Use headings and bullets to break up text. Be sure to leave plenty of white space around the margins and between sections.
| Remember Refer to the Office of Management and Budget (OMB) Policies for Federal Public Websites for further guidance. |
Many of the elements that improve written and oral communication can be applied to online information, including using plain language, large font, white space, and simple graphics.7 Other elements are specific to the Internet. These include:
Enhancing text with video or audio files
Including interactive features and personalized content
Using uniform navigation
Organizing information to minimize searching and scrolling6
Giving users the option to navigate from simple to complex information
A critical way to make information on the Internet more accessible to persons with limited literacy and health literacy skills is to apply user-centered design principles and conduct usability testing.
Usability
is a measure of several factors that affect a user's
experience interacting with a product, such as a
Web page. These
factors include:
To learn more about usability, visit www.usability.gov. |
Ask questions using the words “what” or “how” instead of those that can be answered with “yes” or “no.” For example, “Tell me about your problem. What may have caused it?”3 Try asking “What questions do you have?” instead of “Do you have any questions?”
Plain English will not necessarily help individuals who do not speak English as their primary language and who have limited ability to speak or understand English. To better ensure understanding, health information for people with limited English proficiency needs to be communicated plainly in their primary language, using words and examples that make the information relevant to their potentially different cultural norms and values.
The “teach-back” method is a technique that healthcare providers and consumers can use to enhance communication with each other. The person receiving the health information is asked to restate it in their own words—not just repeat it—to ensure that the message is understood and remembered. When understanding is not accurate or complete, the sender repeats the process until the receiver is able to restate the information needed.8 Consumers also can be asked to act out a medication regimen.3
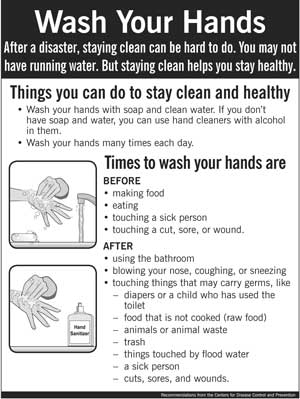
Easy-to-read flyer developed by the Centers for Disease Control and Prevention. The flyer was developed in multiple languages.
| Tip: Checking
for understanding Summarize what the patient needs to do. Consider using a handout or brochure written in plain language. Explain what each medication is for, along with the dosage and side effects. Make sure the patient knows where the information is written down. Then check for understanding: “I want to be sure I didn't leave anything out that I should have told you. Would you tell me what you are to do so that I can be sure you know what is important?” (Source: Doak CC, Doak LG, Root JH. 1996. Teaching Patients With Low Literacy Skills. JB Lippincott Company: Philadelphia, PA.) |
Encourage colleagues to do the same. Consider organizing a training for health professionals and staff in your organization.
| Checklist
for Improving the Usability of Health Information
ϖ Identify the intended users ϖ Use pre- and post-tests ϖ Limit the number of messages ϖ Use plain language ϖ Practice respect ϖ Focus on behavior ϖ Check for understanding ϖ Supplement with pictures ϖ Use a medically trained interpreter or translator |
1National Cancer Institute. Making Health Communication Programs Work. Washington, DC.
2National
Institute of Deafness and Other Communication Disorders.
Improving Health Literacy. Available at http://www.nidcd.nih.gov/
about/what.asp.
3Doak C, Doak L, Root J. 1996. Teaching Patients With Low Literacy Skills. 2nd Edition. JB Lippincott Co.: Philadelphia, PA.
4Plain Language Action and Information Network. Available at www.plainlanguage.gov. Accessed on October 21, 2005.
5American Institute for Research. 1981. Guidelines for Document Designers. Washington, DC.
6U.S. Department of Health and Human Services. Usability Basics. Available at http://www.usability.gov/basics/index.html. Accessed on October 13, 2005.
7Baur CE. 2005. Using the Internet To Move Beyond the Brochure and Improve Health Literacy. In Understanding Health Literacy. Schwartzberg JG, VanGeest JB, Wang CC, Editors. AMA Press, 141-154.
8Schillinger D, Piette J, Grumbach K, Wang F, Wilson C, Daher C, Leong-Grotz K, Castro C, Bindman AB. 2003. Closing the loop: Physician communication with diabetic patients who have low health literacy. Archives of Internal Medicine. 163(1): 83-90.
RESOURCES
| To Learn More About Health Literacy |
Health Literacy: A Prescription
to End Confusion
Released in 2004 by the Institute of Medicine (IOM),
this report examines the body of knowledge that applies
to the field of health literacy and recommends actions
to promote a health-literate society.
Available at: www.iom.edu/report.asp?id=19723
![]()
Healthy People 2010
Healthy People 2010 is a comprehensive set of
disease prevention and health promotion objectives developed
to improve the health of the nation. Objectives 11-2
and 11-6 specifically address health literacy.
Available at: www.healthypeople.gov/Document/HTML/Volume1/11HealthCom.htm
The Health Literacy of America's
Adults: Results from the 2003 National Assessment of Adult Literacy
(NAAL)
This report is the first release of the NAAL health literacy
results. The results are based on assessment tasks designed
specifically to measure the health literacy of adults living in the
United States. Health literacy was reported using four
performance levels: Below Basic, Basic, Intermediate and Proficient.
Available at:
http://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2006483
Communicating Health:
Priorities and Strategies for Progress
This publication provides in-depth action plans for each
of the six Healthy People 2010 Health Communication
Objectives, including Objectives 11-2 and 11-6 on health
literacy.
Available at: http://odphp.osophs.dhhs.gov/projects/HealthComm/
Literacy and Health
Outcomes
This report from the Agency for Healthcare Research and
Quality (AHRQ) provides a systematic review of the literature
on literacy, its relationship to various health outcomes
and disparities, and the effectiveness of health literacy
interventions.
Available at: www.ahrq.gov/clinic/epcsums/litsum.htm
Bibliography Understanding
Health Literacy and Its Barriers
The National Library of Medicine's (NLM) bibliography
provides a comprehensive list of health literacy citations
from varying disciplines and publications. The bibliography
is divided into specific topic areas.
Available at: www.nlm.nih.gov/pubs/cbm/healthliteracybarriers.html
Scientific and Technical
Information: Simply Put
This guide from the Centers for Disease Control and Prevention
(CDC) will help you translate complicated scientific
and technical information into material that captures
and keeps the interest of your intended audience.
Available at:
http://www.cdc.gov/od/oc/simpput.pdf
CDCynergy (CD-ROM)
A multimedia CD-ROM used for planning, managing, and
evaluating public health communication programs. The
planning model is designed to guide the user through
systematically conceptualizing, planning, developing,
testing, implementing, and evaluating health communication
activities, while promoting accountability and the importance
of evaluation.
Available at:
http://www.cdc.gov/healthmarketing/cdcynergy
Making Health Communication
Programs Work (the “Pink Book”)
The planning steps in this guide from the National Cancer
Institute (NCI) can help make any communication program
work, regardless of size, topic, intended audience, or
budget. The Pink Book describes a practical approach
for planning and implementing health communication efforts.
Available at: www.cancer.gov/pinkbook
Plainlanguage.gov
Designed to improve communication from the Federal Government
to the public, this Web site contains excellent tools
and examples of plain language.
Visit http://www.plainlanguage.gov
A Family Physician's
Practical Guide to Culturally Competent Care
This guide, developed by the Office of Minority Health
(OMH), includes cultural competency curriculum modules
designed to equip family physicians with awareness, knowledge,
and skills in cultural competency to better treat the
increasingly diverse U.S. population.
Available at: http://cccm.thinkculturalhealth.org
![]()
National Standards for Culturally
and Linguistically Appropriate Services in Health Care
OMH has developed comprehensive standards on culturally
and linguistically appropriate services (CLAS) in health
care. The CLAS standards provide definitions of culturally
and linguistically appropriate services and address organizational
structures and policies that help healthcare professionals
respond to cultural and linguistic issues presented by
diverse populations.
Available at: www.omhrc.gov/assets/pdf/checked/finalreport.pdf
Policies for Federal
Public Websites
The Office of Management and Budget issued the Policies
for Federal Public Websites in 2004. The policies
are designed to improve the usability of Federal Web
sites.
Available at:
http://www.usa.gov/webcontent/reqs_bestpractices/omb_policies.shtml
Usability.gov
A resource for usable, useful, and accessible Web sites.
This site contains information, guidelines, and checklists
for conducting usability testing and user-centered design.
Visit www.usability.gov
Improving Patient Safety
Through Informed Consent for Patients With Limited Health
Literacy
This report, from the National Quality Forum, is designed
to provide an overview of major issues involved in providing
informed consent for all patients, particularly those
with limited health literacy.
Available at:
http://www.qualityforum.org/pdf/reports/informed_consent.pdf
![]()
Understanding Health
Literacy
This comprehensive resource of health literacy research
seeks to improve understanding of this public health
challenge and to stimulate research focused on reducing
or eliminating the literacy barrier to effective medical
diagnosis and treatment. The book includes a chapter
on the literacy demands of healthcare settings.
Citation: Schwartzberg JG, VanGeest JB, Wang CC, Editors.
Understanding Health Literacy. AMA Press. 2005.
Consumers in Health
Care: The Burden of Choice
This report by the California HealthCare Foundation presents
the latest research on consumer decisionmaking, explores
the methods consumers use to make choices, and looks
at what influences affect consumer action. The research
suggests important implications for the development of
effective information tools for consumers.
Available at: www.chcf.org/topics/view.cfm?itemid=115327
![]()
healthfinder®
healthfinder® is an award-winning Federal Web site
for consumers, developed by the U.S. Department of Health
and Human Services and other Federal agencies. Since
1997, healthfinder® has been recognized as a key
resource for finding the best government and nonprofit
health and human services information on the Internet.
healthfinder® links to carefully selected information
and Web sites from more than 1,500 health-related organizations.
Available at: www.healthfinder.gov