ARTICLE #11: Treatment Options for Spasticity Causes and EffectsWith normal muscle function, opposite muscles work in opposite directions. This means that when one muscle pulls or contracts, the other relaxes. Spasticity is a condition which occurs when muscles opposite each other both contract or relax at the same time. Spasticity is a common symptom of MS. Resulting from demyelination along the nerves that control muscle tone, spasticity causes a tightening of the muscles. With MS, spasticity most frequently affects the different muscles of the legs, buttocks, back, and arms. For some, spasticity can be mild, causing no real discomfort or inconvenience. Mild spasticity even provides some benefits, such as improving circulation, helping to prevent blood clots, maintaining muscle tone, and decreasing leg weakness. Muscle stiffness can provide added support while an individual is standing, walking, or transferring from one spot to another. Unfortunately, many individuals with MS experience moderate to severe spasticity. This can be a debilitating symptom, which can greatly limit movement, use up valuable energy, and become quite painful. Another form of spasticity occurs in episodes, often at night. These are unexpected, involuntary movements of the leg (or sometimes the arm) where the limb suddenly draws up into a clenched position, or kicks out into an extended position. Spasticity, when combined with weakness, can lead to contractures as well. This is when the tendons are tight and the joint is difficult to move; it can even become locked in one position. In addition to pain and immobility, complications of contractures include an increased risk of pressure sores, pneumonia, urinary tract infections, and generalized debilitation. When spasticity is successfully treated, tight muscles relax, restoring movement and reducing pain. While many treatment options are available for spasticity, physicians continue to look to new drug and therapy combinations for optimal treatment plans. Therapies and DevicesTreatment begins by regularly seeking help for any other health conditions that may aggravate or intensify spasticity and its painful effects. Such conditions can include infections, as well as anything worn that doesn't fit properly, such as a brace, cast, or tight clothing. The next lines of treatment are stretching exercises and physical therapy. Stretching exercises can be very effective in relieving symptoms of spasticity, and these are typically performed while sitting or lying down, allowing gravity to assist with the stretching. A physical therapist can create a customized exercise program for an individual to perform daily at his or her home. Devices or mechanical aids are another type of treatment to relieve spasticity and reduce the risk of contractures. The physical therapist can design a custom brace, splint, toe or finger spreaders, or other device to hold an affected area in position. Contractures are sometimes treated through a series of casts which progressively stretch the tendons around a joint to promote greater movement. Medications and Other OptionsThe most commonly prescribed drug for spasticity in MS is oral baclofen. This drug works well for a number of people, but dose must be carefully monitored. Too little of this drug can prove to be ineffective, while too much causes muscle weakness, fatigue, and confusion. Drowsiness and nausea are other side effects of this medication. Baclofen may not be abruptly discontinued as serious problems such as seizures may result. Tizanidine (Zanaflex®) is another drug frequently prescribed for spasticity. Dose titration (building gradually to a full dose) is important to reduce sedation. The combination of baclofen and tizanidine is feasible if done cautiously to avoid side effects. If baclofen or tizanidine is not successful or well tolerated, other types of drugs may be used to treat spasticity and spasms in MS. These include muscle relaxants, anti-epileptic medications, and certain sedatives. Many cause drowsiness, so some may be more appropriate at nighttime. These medications include: sodium dantrolene (Dantrium ®); clonazepam (Klonopin®); diazepam (Valium®); gabapentin (Neurontin®); carbamazepine (Tegretol®); cyclobenzaprine HCl (Flexeril®); methocarbamol (Robaxin®); L-dopa (Sinemet®); and selegiline (Eldepryl®). Another option for treating spasticity is botulinum toxin A (Botox®) injections. While initially used for treating small areas such as the face or eye, Botox has since been shown to be very useful for localized areas of spasticity in the limbs. Bladder spasticity is sometimes treated with Botox as well. Please note that Botox, as well as other treatments for spasticity, may have potential adverse side effects. Individuals are advised to consult a physician about any potential risks before starting a new treatment. More severe procedures, such as blocking the nerve permanently (through injecting phenol into a muscle or by surgically cutting the nerve) can result in flaccidity, which is a significantly loose muscle. While these procedures reduce or eliminate spasticity, spasms, and pain, they do not increase mobility and also carry risks. Intrathecal Baclofen Therapy
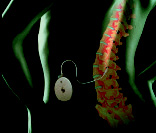
Individuals with MS who are suffering from severe spasticity will often experience a significant improvement after receiving a baclofen pump. While an individual will not gain back lost function resulting from demyelination, he or she will get back any ability that was prevented due to spasticity. Moving, walking, transferring, activities of daily living, sleeping, and personal care can all be dramatically improved if spasticity has been the problem. ITB™ Therapy is available through Medtronic®, Inc. As with any surgical procedure, some risks are involved that need to be considered before making a decision. For more information, individuals are advised to consult their physician. Readers may also go to www.spasticity.com , or contact Medtronic by calling (800) 328-0810. Please note that MSAA does not endorse or recommend any specific product, medication, or procedure. All details given are for informational purposes only; all decisions regarding changes in treatment should be made under the guidance of a qualified physician. For more information about spasticity, please visit msassociation.org/programs/videos for an online MSi video presentation on spasticity, given by Dr. Donald Barone. Readers may also speak with an MSAA Helpline consultant by calling (800) 532-7667 |